Red blood cell antigens are best known as A, B,
AB, and O, however, up to 342 identified independent antigens can be present on
a single red blood cell.1 The present antigens on an individual’s
red blood cells are recognized and processed by their immune system as
originating from themselves.5 When an antigen that is not typically
present is found by an immune cell, the immune system deems the red blood cell
as foreign and proceeds to attack it and others with the same antigen.5
For this reason, when an individual needs a blood transfusion, they must
receive their donation from someone who has compatible antigens on their red
blood cells.5 This can become difficult when the individual has a
more rare pattern of blood antigens on their blood cells or in other words, a
rare blood type.
 |
| Figure 1. The common blood types with their coinciding alloantibodies. |
When blood types such as A or AB are discussed,
they are mentioned in the context of if the individual is positive or negative
for them. When the individual is negative for the antigen, they can donate to
an individual that is positive or negative for the antigen but can only receive
a donation from an individual negative for it.5 The most discussed
blood types are A+, B+, AB+, O+, A-, B-, AB-, and O-.5 The most well
recognized flexible blood donor group is O- which is known as the universal
donor because they are able to donate to all previously mentioned blood types.5
The most widely compatible blood group is known as golden blood and individuals
with this extremely rare blood type are inherently able to donate to all rare
blood types from the Rh antigen system and even common blood types.6,11
Rh-deficiency syndrome, an autosomal recessive
genetic disorder characterized by red blood cells that lack all 61 antigens
known as Rh system antigens, can occur in both a complete (Rhnull) or
significantly reduced phenotype (Rhmod) .2,6 The syndrome is
extremely rare, it has been reported less than 50 times since its discovery in
1960.11 Other rare blood types from the Rh antigen system can lack
any one or more of the Rh antigens but less than all. The low prevalence of the
Rhnull phenotype and the potential complexity of the other Rh system blood
types makes finding a blood donor for a patient with these blood types extremely
hard. This is where the coined term ‘golden blood’ is derived. Afflicted
individuals are classified into two subgroups based on their specific genetic
defect; regulatory when the mutation is in a suppressor gene and amorph when it
is at the Rh gene locus.2,9 Patients with Rhnull syndrome are found
to have stomatocytes which are osmotically fragile red blood cells that undergo
hemolysis when in a hypotonic environment.2,3,8 This is a result of
their abnormal shape that seems to coincide with the lack of the cell membrane
antigens.3 As a result of this the patients also suffer from chronic
hemolytic anemia to some degree.2,3 This is a condition in which the
patients’ blood cells are broken down via hemolysis faster than they are made.7
Individuals with hemolytic anemia have symptoms such as fatigue, pale
skin, chills, fever, heart palpitations, confusion, and more.10 Clinically
Rh deficient patients readily produce alloantibodies when exposed to Rh
antigens and in certain situations such as pregnancy can be very dangerous.2,4
 |
| Figure 2. Stomatocytes in culture. |
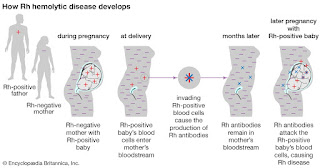
When a Rhnull mother is pregnant with a fetus
with the Rh antigens (Rh+) the mother's immune system may create antibodies
against the fetus’s red blood cells and destroy them.1 This can
cause hemolytic anemia in the fetus and the severity of the anemia can induce
brain damage, severe illness, or even death of the fetus.1 Expecting
mothers whose red blood cells are lacking any of the Rh system antigens and
have not yet produced antibodies towards her growing fetus may be put on Rh
immunoglobulin (Rhlg) at around the 28th week of pregnancy.1
This can prevent the mother from starting to produce antibodies to the fetal
blood cells for the remainder of the pregnancy.1 The mother is also
given another dose of the Rhlg post-birth to prevent any Rh+ cells left in the
mother from producing an immunological reaction.1 Any Rh- mothers
that produced antibodies to Rh+ fetal blood will not be helped by Rhlg
treatment.1 While this condition may only affect a select few
expecting mothers however, it can make their pregnancy very difficult and
scary.
 |
| Figure 3. Illustration of fetal hemolytic disease development |
As previously mentioned, individuals with
golden blood are able to donate to anyone with common or specific rare Rh
system blood types without their blood generating an immune response in the
recipient.6 Before Rhnull blood was first discovered it was thought
an individual without these antigens would not survive utero.6 Since
its discovery, golden blood has been sought after by researchers and physicians
alike for its rare properties, however, in 2017 there were only 9 active
donors.11 This makes finding a single bag of the blood extremely
difficult which has made blood transfusions for these patients complicated and
slowed the progression of studies on the blood.11 Despite
this, with all of its very special characterizations, these individuals’ blood
holds an extraordinary place in the healthcare and scientific communities.6
References:
1. Rh Factor. American Pregnancy
Association. https://americanpregnancy.org/pregnancy-complications/rh-factor/.
Published October 9, 2019.
2. Journal Of Pakistan Medical
Association. JPMA. https://jpma.org.pk/article-details/2399.
3.
Stomatocyte. Stomatocyte - an
overview | ScienceDirect Topics.
https://www.sciencedirect.com/topics/medicine-and-dentistry/stomatocyte.
4.
Glossary: Alloantibody - Blood Bank
Guy Glossary. Blood Bank Guy. https://www.bbguy.org/education/glossary/gla17/.
5.
Blood: the basics. Professional
Education.
https://professionaleducation.blood.ca/en/transfusion/publications/blood-basics.
Published February 11, 2019.
6. Bailey P. Wellcome. The man with the
golden blood. https://mosaicscience.com/story/man-golden-blood/.
7.
Hemolytic Anemia. Johns Hopkins
Medicine.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/hemolytic-anemia.
8.
Osmotic fragility test:
MedlinePlus Medical Encyclopedia. MedlinePlus.
https://medlineplus.gov/ency/article/003641.htm.
9. Cartron, Jean-Pierre.
"Rh-deficiency syndrome." The Lancet 358 (2001):
S57.
10.
Hemolytic Anemia. National Heart
Lung and Blood Institute.
https://www.nhlbi.nih.gov/health-topics/hemolytic-anemia.
11.
Rhnull, the Rarest Blood Type on
Earth, Has Been Called the "Golden Blood". Curiosity.com.
https://curiosity.com/topics/rhnull-the-rarest-blood-type-on-earth-has-been-called-the-golden-blood-curiosity/.
By Cheyenne Cook, A Master’s of Medical
Sciences Student at the University of Kentucky

Very interesting blog post, we all know that O neg is the universal blood donor and The RhD protein refers to one of 61 potential proteins in the Rh system. Blood is considered Rh-null if it lacks all of the 61 possible antigens in the Rh system. golden blood is incredibly important to medicine, but also very dangerous to live with. If a Rh-null carrier needs a blood transfusion, they can find it difficult to locate a donor, and blood is notoriously difficult to transport internationally. Rh-null carriers are encouraged to donate blood as insurance for themselves, but with so few donors spread out over the world and limits on how often they can donate and is extremely hard to give up golden blood because of this extreme shortage.
ReplyDeleteCheyenne, very interesting post! Although I am of course familiar with blood typing systems and the various associated surface antigens, I have never heard of the "golden blood" phenotype before. I can't think of another phenomenon in medicine that is as rare as that, which makes it particularly fascinating.
ReplyDeleteRh factor incompatibility between a mother and fetus is frightening but thankfully modern medicine allows us to handle that scenario routinely with little trouble. Hopefully in the future molecular biomedical techniques will advanced to a point where cell surface antigens can be easily manipulated and/or reproduced, with special emphasis on self vs. non-self recognition by the host immune system such that complications as you mentioned can be easily overcome.
Great post!
Wow, very interesting! I have never heard of the golden blood donor, much less the complications from Rh deficiencies. It's scary to think that some people have a very limited supply of donor blood available to them in case of an emergency. However, I wonder if it would be possible to administer Rh immunoglobulin to Rh null patients to allow for blood transfusions, similar to the way they administer RhIg to Rh deficient pregnant mothers. I am also interested to see whether gene therapy could help Rh deficient patients since you mentioned that both types originate from a gene mutation. Very cool topic.
ReplyDeleteVery interesting blog! I knew from before that blood transfusion was difficult as it is. However, I was completely unaware of the consequences of a Rhnull mother having a Rh antigen fetus. We are always told that the donor blood is the best type, but we are unaware of the effects the individual has to deal with. It is like a blessing for others, but a curse for the person with golden blood. It is understandable that there are a few number of individuals with this blood type and an even a smaller number of people who want to donate this blood type.
ReplyDeleteI looked into an article on how pig’s blood is being engineered to be compatible with human blood, however that is still a far goal in our medical field due to multiple reasonings. The most difficult and important reasoning is getting human trials since there is not really another way to get the interaction of human blood antigens with pig’s blood antigens. It could be done in a controlled environment but that does not provide the individuality that each human body and its unique response could.
Li, Ping et al. “The potential role of 3D-bioprinting in xenotransplantation.” Current opinion in organ transplantation vol. 24,5 (2019): 547-554. doi:10.1097/MOT.0000000000000684
https://www.ncbi.nlm.nih.gov/pubmed/30711308
I, too, have never heard of "golden blood" prior to your blog. I guess that easily attests to the rarity of this blood type. It also shows how much more we have to learn and explore in the realm of medicine. As others have mentioned, the limited availability of this blood type can pose complications in an urgent situation. At the same time because of how rare this is, it would likewise be rare that it is needed. With the constant chatter of gene manipulation and so forth, I am curious to see how medicine might evolve towards possibly manipulating the surface antigens. We all bleed red and yet are so different!
ReplyDeleteJen Eccleston
This topic is something that I had heard about but never looked into. I enjoyed getting the information about what "golden blood" is and how it is so rare. It was very interesting to read how Rh factors play such an important role. The rarity of this Rh factor being null in golden blood was interesting to read about. I was wondering if scientists could use this blood to test certain diseases and see what the results would be. Also due to the Rh factor being null, I wonder if it is possible for researchers to possible create this blood in a lab and help these rare people?
ReplyDeleteThe Rh factor is something that many don’t know about and wouldn’t unless they got pregnant. A mother that is Rh negative is susceptible to creating antigens to her baby is the baby is Rh positive. This is only a problem when the second baby is also Rh positive. Because of this exchange of blood in utero and at birth the mom will produce antigens to attack the second fetus producing fetal hemolytic disease of the newborn. This is why mothers are given Rhogam before the baby is born. I have not heard about Rh-deficiency syndrome and did not realize there are people with “golden blood.” How would an individual find out that they have this disease? And do you think that removing blood periodically to save for future problems is a good idea? Almost like blood doping but instead its like a back up plan incase the individual need a transfusion.
ReplyDelete-Erin Harris
DeleteThis is something that I've learned about, but I never revisited the topic. This is really interesting and good to think about in medicine, because a patient could be decompensating and this would be crucial to know when treating them. Saving the blood for future issues could/will be huge for that patient or others. If they knew they had "golden blood," they could periodically donate. Very interesting.
ReplyDeleteThis comment has been removed by the author.
ReplyDeleteYour topic was so interesting! I can honestly say that I have never heard of ‘golden blood’. I have always wondered how the mechanisms of blood transfusions work, but you explained this very well in your post. I am fascinated that an individual can benefit from another person’s blood when they are in need of it. I love that Rh-null carriers are able to donate blood that can be used for any other blood type. I think the difficult part about this, is that only another Rh-null carrier could donate blood to another Rh-null carrier. Your blog post written very well and was extremely informative! Great job.
ReplyDeleteVery interesting post. I had actually never heard of the term golden blood and this is quite interesting, and very well described in your blog. As having the O- blood type myself, I have been informed about the necessity of blood donation for as long as I can remember. When working in the Emergency Department, I watched thousands of units of blood be administered. Being the universal donor blood, it is also known that there is never enough, as so many trauma patients receive it when in an emergency situation. That does lead to worry for those individuals who can only receive O-blood. I think the take away from this, especially for our young, somewhat healthy age group is to one, know your blood type, and two do your part to donate as often as possible.
ReplyDeleteWow, this is the first blog post where I have learned something totally new! Golden blood is something I have never heard of before, however it is a very interesting disorder. Rh-null being the ultimate donor is very interesting, it is fascinating when a disorder can present so many benefits for the population at large. This blog post is extremely good, great work!
ReplyDeleteWonderful post, Cheyenne. You did a good job giving a concise yet thorough background regarding blood and Rh deficiency syndrome. I do wonder, though, if the rarity of golden blood could potentially lead to medical professionals seeking the blood in an unethical manner. In particular, I'm thinking of Henrietta Lacks and how even after her death, scientists kept pressuring family members to donate blood or come in for testing to discover more about her cells. While the times have changed, I wonder if the 9 active donors may be sought after in the hopes of helping others. Overall, great job!
ReplyDeleteCheyenne, very interesting topic! I was my mother’s second child; both my older sister and I are Rh+ but my mom is Rh-. Thankfully, the doctors were able to treat my mother while she was pregnant. She was given an injection twice with what she described as a Rh vaccine, which would prevent my antibodies from harming either of us. I wonder if there could be a way of modifying blood cells to be Rhnull, because with only nine active donors I would worry what would happen in an emergency and those people were not available. I also wonder if there are other beneficial health characteristics this rare blood type offers.
ReplyDeleteNiamh Costello
I really enjoyed this post Cheyenne! I always knew that O- blood could be used as an universal donor, but I never knew about the Rh-deficiency syndrome in humans. This issue is huge in the equine industry and something I learned extensively about from an equine veterinarian I shadowed at one point. Her main frustration with the syndrome is that it’s so easy to test for, but most owner’s do not want to pay the comparatively cheap cost for the testing to be done. I would really like to know more about the fetal stage in humans, and the comparisons between the equine and human form. Maybe this could help provide some more information towards the human syndrome!
ReplyDeleteThis is so cool! I never knew about this Rh deficiency. It reminds me of the specificity of matching HLA for organ transplants. I am intrigued by the possibility of creating synthetic blood, in the same way that they are attempting to 3D print and grow synthetic organs from a patient's own stem cells. Perhaps this could be a possible solution to the problem of few donors for patients with this "golden blood". With new technological developments, hopefully these people will no longer be in as much danger from the lack of viable blood to transfuse when they are sick or injured.
ReplyDeleteWoah, Cheyenne, this is a very interesting blog post for many reasons. I had no idea that such a serious condition existed and necessitated such a special type of blood. It is especially interesting and concerning that there are only a handful of donors contributing their blood for treatment of this disease; truly this blood must be more valuable than gold, hence its name. Are there any other options for treating this Rh blood type with either drugs or gene therapy? Rather, are there any ways to produce this golden blood artificially by modifying donated blood or seeking another, perhaps animal, source.
ReplyDeleteGreat explanation of the different blood types and Rh deficiency syndrome. I had very little knowledge of this disease and you taught me a lot. I was under the impression that this disease was only caused by mutations at the Rh gene locus, I was not aware that there could be a mutation in the gene that encoded the suppressor of the Rh gene as well. I wonder if a potential treatment for these rare individuals could be something similar to a cancer immunotherapy technique that use MHC cells to introduce a viral vector to the body so that the immune system recognizes it as "self" and the recombinant virus is free to replicate it's DNA and hijack cell machinery to produce anti-cancer antigens without being wiped out. I would be interested to see if the technique can be modified so that the MHC cell instead can introduce Rh proteins as friendlies to the immune system prior to a blood transfusion, preventing any sort of detrimental immune reaction. Another thought is that this could also be a potential scenario where Cas9 could help remedy the mutation.
ReplyDeleteGreat post! I was completely ignorant to this phenotype before reading your post. Blood transfusion services might face challenges in providing compatible blood for patients with red blood cells lacking high-incidence antigens and who have made the corresponding alloantibody. A hospital blood bank should have a written protocol in place, explaining what needs to be done for rare blood request. In this event, providing blood for a patient whose antibodies reacted with RBCs of all available ABO compatible units, management of the time with quick response along with a sound clinical and laboratory judgment are necessary to save the patient’s life. Availability of a National Rare Donor Program and support of well-trained reference laboratory personnel in a close collaboration with relevant medical team help to manage a patient’s need to a very rare Rhnull phenotype in an acceptable turnaround time. Consanguineous marriage plays an important role in the creation of this type of blood group, so it may be prudent for researchers to look specifically in the regions to search for potential donors. Very interesting post overall!
ReplyDelete1. Shahverdi, Ehsan et al. “First Report of Known Rare Rhnull Phenotype Individuals in Iran.” International journal of hematology-oncology and stem cell research vol. 12,3 (2018): 181-184.
Very efficiently written information. It will be beneficial to anybody who utilizes it, including me.
ReplyDeleteblood dyscrasia meaning